
 |
|
Priscila Mina Falsarella; Rafael Dahmer Rocha; Antonio Rahal Junior; Guilherme Falleiros Mendes; Rodrigo Gobbo Garcia
ABSTRACT
OBJECTIVE: To analyze the efficacy of recombinant tissue plasminogen activator (r-TPA) injection in the evolution of percutaneous drainage of thick collections. MATERIALS AND METHODS: This was a single-center study involving the retrospective analysis of hospitalized patients undergoing percutaneous drainage of thick (superficial or intracavitary) fluid collections, followed by injection of a fibrinolytic agent (r-TPA) into the affected space. RESULTS: A total of 53 percutaneous drainage procedures, with r-TPA injection, were performed in 51 patients. Abdominal and pelvic collections were the most common, being seen in 38 (73%) of the procedures; in 35 (66%), the etiology of the collection was attributed to postoperative complications. A total of 61 catheters were used in order to drain the 53 collections. Of those 61 catheters, 52 (85%) were large (12–16 Fr) and 9 (15%) were small (4–10 Fr). The mean r-TPA dose was 5.7 mg/collection per day, and the mean time from r-TPA injection to drain removal was 7.7 days. Percutaneous drainage in combination with r-TPA injection was successful in 96% of the cases. None of the patients showed coagulation changes during the study period. CONCLUSION: The use of once-daily, low-dose r-TPA for up to three consecutive days, as an adjunct to percutaneous drainage of thick collections, with or without loculation, appears to be an effective technique.
Keywords: Abscess; Drainage; Fibrinolytic agents.
RESUMO
OBJETIVO: Analisar a eficácia da injeção do agente fibrinolítico ativador tissular de plasminogênio (r-TPA) na evolução da drenagem percutânea de coleções espessas. MATERIAIS E MÉTODOS: Estudo unicêntrico com análise retrospectiva de pacientes internados submetidos a drenagem percutânea de coleções espessas, superficiais ou intracavitárias, seguida da injeção de agente fibrinolítico (r-TPA) no interior da coleção. RESULTADOS: Foram realizadas 53 drenagens percutâneas com injeção de r-TPA em 51 pacientes. Coleções intra-abdominais e pélvicas foram as mais frequentes (n = 38; 73%) e a causa predominante foi complicação pós-operatória (n = 35; 66%). Foram utilizados 61 drenos para acessar as 53 coleções, dos quais 52 (85%) foram drenos mais calibrosos (12–16 Fr) e 9 (15%) de pequeno calibre (4–10 Fr). A dose média de r-TPA empregada foi 5,7 mg/coleção/dia, o tempo médio entre a injeção de r-TPA e a retirada do dreno foi 7.7 dias e o sucesso da drenagem percutânea em associação com agente fibrinolítico foi observado em 96% dos casos. Alterações de coagulação não foram observadas nos pacientes durante o estudo. CONCLUSÃO: O uso de baixas doses diárias de r-TPA por até três dias consecutivos, como adjuvante terapêutico na drenagem percutânea de coleções espessas e/ou loculadas, demonstrou ser uma técnica efetiva.
Palavras-chave: Abscesso; Drenagem; Fibrinolíticos.
INTRODUCTION Complex collections typically present a therapeutic challenge and can range from organized collections of blood with locoregional compressive symptoms to infectious processes that, in patients with various comorbidities, can result in unfavorable clinical outcomes such as sepsis and death(1). Complicated infection is a major cause of high morbidity and mortality, occurring most commonly in the abdominal cavity—in approximately 30% of cases(1)—and thoracic cavity—in 18–60%(2). Among the main factors associated with a worse prognosis are worsening of severe underlying diseases, failure to determine the etiology of the collection, the use of inappropriate empirical antibiotic therapy, and infections caused by multidrug-resistant organisms. Early diagnosis, as well as the introduction of aggressive clinical and surgical therapies, are key to achieving favorable clinical outcomes(1). Minimally invasive percutaneous drainage guided by imaging, such as ultrasound and tomography, which are frequently used in conjunction(3), is a well-established therapeutic option in the approach to collections at various sites, such as subcutaneous collections, as well as those in the intramuscular compartment, abdomen/pelvic cavity, and thorax(3–6). The advent of imaging equipment that provide better definition and various types of drains (to deal with superficial and deep collections of different viscosities) have resulted in an increase in the number of cases in which the minimally invasive technique is indicated, as well as improving outcomes. However, in thick, septated, encapsulated collections of blood containing debris, the minimally invasive approach provides less than satisfactory results(7–9). In this context, the injection of fibrinolytic agents into the collection, in order to reduce the viscosity of the contents and facilitate the flow through the lumina of drainage tubes of different calibers(10,11), represents a solution for the treatment of these less common cases in which the success of minimally invasive drainage is limited(8,9,12), precluding the need for a more aggressive surgical approach, which is sometimes not applicable in patients who are more seriously ill. The objective of this study was to analyze the safety and efficacy of recombinant tissue plasminogen activator (r-TPA) injection in the evolution of imaging-guided percutaneous drainage of thick fluid collections. We also describe the initial experience of the interventional radiology department of our hospital in the application of the technique. MATERIALS AND METHODS This was a single-center study involving the retrospective analysis of patients submitted to percutaneous drainage of thick superficial or intracavitary fluid collections, followed by injection of a fibrinolytic agent, between April 2011 and May 2015. This study was approved by the medical ethics committee of the institution. Administration of r-TPA The decision to use the fibrinolytic agent was made jointly between the interventional radiology team and the members of the clinical-surgical treatment team assigned to the patient. After the appropriate positioning of the percutaneous drain had been verified by imaging, the fibrinolytic agent was injected through the lumen of the drain. The r-TPA was diluted in saline solution (ranging from 10 mL to 40 mL depending on the estimated initial volume of the collection) and instilled within the collection, with subsequent closure of the drain for 1 h. Subsequently, the drain was opened and the flow rate was measured, the measurement excluding the volume of solution administered. The treatment cycle consisted of administration of a daily dose of the saline-r-TPA solution for three consecutive days, unless the collection resolved spontaneously before that period. During administration of the fibrinolytic agent, the serum fibrinogen level was monitored and a coagulation test was performed. RESULTS Percutaneous drainage of superficial or intracavitary collections, with r-TPA injection, was performed 53 times in 51 patients, two patients undergoing drainage of two different collections each. Of the 51 patients, 30 (58.8%) were women. The mean age of the patients was 55.6 years (range, 17–93 years). Abdominal and pelvic collections were the most common (n = 38; 73%), followed by thoracic collections (n = 8; 15%) and collections in soft tissue (n = 7; 12%). The predominant cause of the collections was postoperative complications (n = 35; 66%), followed by pneumonia evolving to empyema (n = 8), liver abscess (n = 2), trauma (n = 2), complicated pancreatitis (n = 1), pyelonephritis (n = 1), renal cyst rupture (n = 1), loculated ascites associated with carcinomatosis (n = 1), and hematoma of the abdominal wall. Drainage was performed with general anesthesia in 25 (49%) of the patients (n = 25), local anesthesia in 18 (35%), and local anesthesia combined with intravenous sedation in 8 (16%). Among the imaging methods used in order to guide the drainage, ultrasound alone was used in 27 (51%) of the procedures, computed tomography alone was used in 8 (15%), and the combination of the two methods was used in 18 (34%). A total of 61 drains were used in order to access the 53 collections (45 were accessed with a single drain and 8 were accessed with two drains per collection). Of the 61 drains, 52 (85%) were large-caliber drains (12–16 Fr) and 9 (15%) were smaller-caliber drains (4–10 Fr). The saline-r-TPA solution was administered after the correct positioning of the drain had been confirmed, being injected immediately after drainage in 28 (53%) of the cases, with a mean interval between the initial drainage and the r-TPA injection of 2.7 ± 4 days (range, 0–13 days). The mean daily dose of r-TPA was 5.7 ± 3.0 mg/collection (range 2–10 mg), with a mean treatment duration of 2.6 days. The mean time between r-TPA injection and drain withdrawal was 7.7 days. There were no changes seen on the coagulation tests evaluated during the study. Among the collections treated with r-TPA injection, the overall success rate of percutaneous drainage in conjunction with the use of a fibrinolytic agent was 96%, successful drainage being achieved in 51 cases, with the following distribution (Figures 1 and 2): after one r-TPA cycle, in 45 cases (85%); after two r-TPA cycles, with resolution of the collection after the second cycle, in 1 (2%); and after placement of a second percutaneous drain in 5 (9%).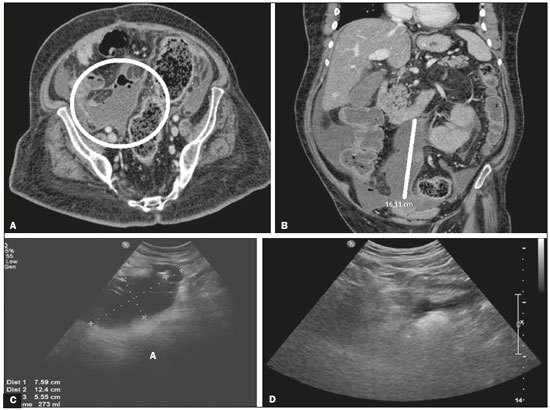 Figure 1. A,B: Computed tomography showing an intraperitoneal collection. C: Ultrasound six days after drainage of the collection, showing septa prior to r-TPA injection. D: Ultrasound three days after the end of the r-TPA cycle, showing resolution of the abdominal collection.
Figure 1. A,B: Computed tomography showing an intraperitoneal collection. C: Ultrasound six days after drainage of the collection, showing septa prior to r-TPA injection. D: Ultrasound three days after the end of the r-TPA cycle, showing resolution of the abdominal collection.
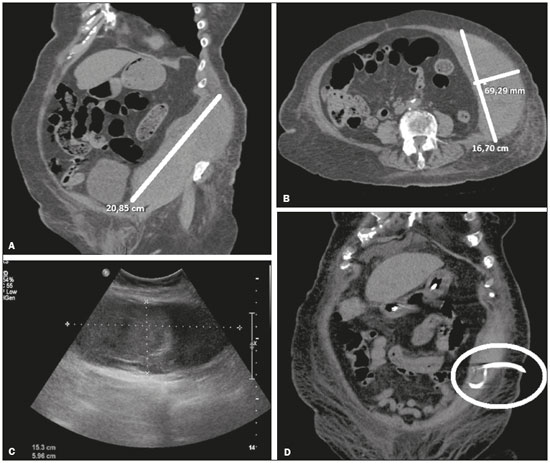 Figure 2. A,B: Computed tomography showing hematoma of the abdominal wall. C: Ultrasound after percutaneous drainage. D: Computed tomography after the end of the r-TPA cycle, showing resolution of the collection.
Figure 2. A,B: Computed tomography showing hematoma of the abdominal wall. C: Ultrasound after percutaneous drainage. D: Computed tomography after the end of the r-TPA cycle, showing resolution of the collection.